The landscape of downtown Toronto is peppered with countless construction sites and – as Canada’s largest city – is home to three million residents, and continues to grow and expand.
Among the hustle and bustle of a thriving downtown, there are pockets of extreme poverty and people who struggle to get by. Over the last 20 years, Toronto has seen an increase in the number of high-poverty neighbourhoods, as well as pockets of poverty in high-income neighbourhoods.
In 2006, a partnership between South Riverdale Community Health Centre, Regent Park Community Health Centre, and Sherbourne Health, with specialist support from Michael Garron Hospital, was formed to help address some of the barriers to accessing hepatitis C care which exist for people living in poverty and who use drugs or alcohol. At the heart of the Toronto Community Hep C Program (TCHCP) are peer-driven support groups, where the emotional and informational support provided are as transformational as treatment.


Until recently, a drug called ‘interferon’ was part of the treatment for hepatitis C. It had significant side effects over a long a period of time and modest cure rates. Many people who used drugs or alcohol were told they could not do treatment. For many people, there seemed no hope for a life without the disease.
In 2015 there was a major change in the hepatitis C treatment landscape with access to new direct-acting antiviral medications. With a 95% cure rate, short treatment durations and minimal side effects, these new treatments offered fresh hope to many that it might be possible to clear hepatitis C. Keith Williams is one of the many TCHCP participants who cleared the virus after taking the new medications.
They told me 24 weeks after I was doing the meds and following it to a tee, they said, ‘Unfortunately it didn’t work.’ I don’t even know how to describe it, it was like a monstrosity. And then somehow, some way, I got the message that there’s another drug coming out and the doctors wanted to talk to me again. And then everything changed, I did that treatment and I was cured.

Keith’s story
A key component of the TCHCP is a commitment to the meaningful involvement of people with lived experience of hepatitis C and drug use. Many of the current program staff, including key community support workers Jennifer Broad and Keith Williams, are former program clients.
Jennifer and Keith are representative of the positive impact the program has on its participants. Over time, the TCHCP has created multiple pathways for clients to build confidence, gain new skills and develop into professionals with valuable experience. Jennifer was recently hired into a full-time role with the program which includes supervising other peer workers and overseeing the program’s peer training program.
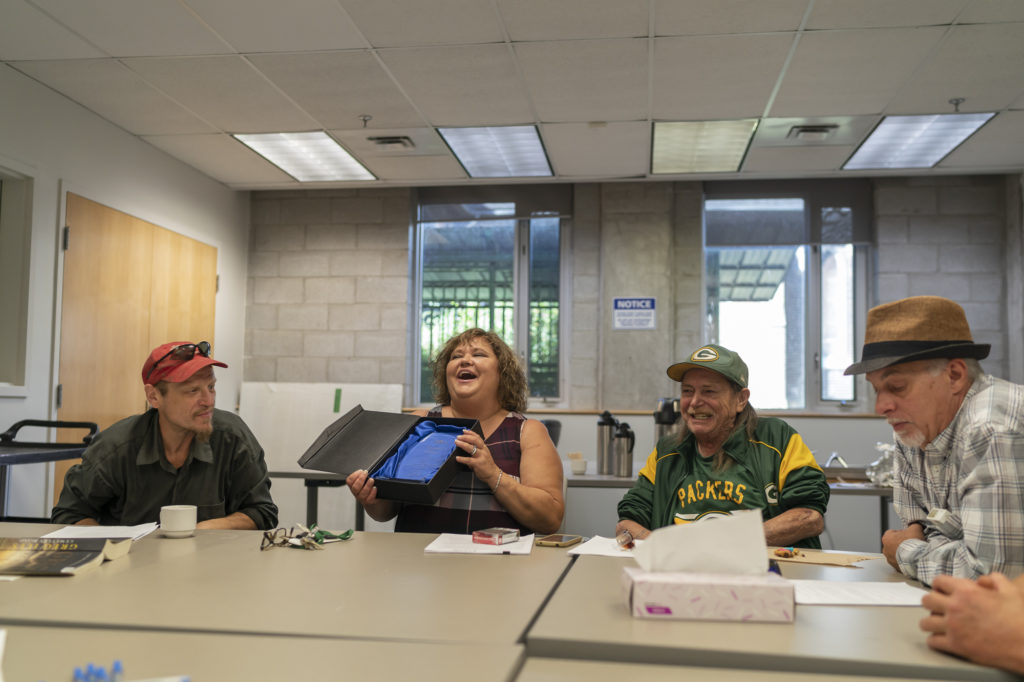
One way this happens is through the Patient Advisory Board, which is made up of clients from each of the program’s sites. The group meets regularly and have helped to co-design aspects of the program and the research it conducts. Another example of participants’ meaningful involvement are the graduates from the TCHCP peer training program who are widely sought out by organisations across the city.
Me and Jen, we’ve been through so much together. Oh man, I love Jen. She was the first person to look at me and say, ‘Keith, you’d be great at this job.’ We work so good together and I’m so glad that I have the team that I do to work with, it makes my job so much easier. She has been there for me since day one.
Rick’s story
South Riverdale Community Health Centre offers comprehensive and multidisciplinary primary care and support to a wide range of community members. It also has a large harm reduction program that includes supervised injection.
TCHCP offers point-of-care RNA testing for hepatitis C as a service embedded in one of their research projects. This was how Rick learned he had hepatitis C. He was immediately connected to the Toronto Community Hep C Program and began attending the weekly groups where clients are offered peer support and education on issues related to hepatitis C and substance use over a warm meal. These regular meetings cultivate relationships between the group members and also develop their personal confidence by highlighting that people’s basic needs and human rights are a priority.
I never knew I had hep C, and then when I got tested, it was like a one-hour wait. Hardly any trouble, a little pinprick and boom I found out I had hep C. Then after that, I started coming to the Hep C Program, and things started looking up and up for me, and things started getting a lot better. Not only that, it’s helped me in so many other ways.
Rick rarely missed his weekly group meetings, and like many other TCHCP participants, he flourished throughout his treatment. Rick developed strong relationships with program staff and also joined the Patient Advisory Board, of which he is now the co-chair.
Two weeks after completing his three-month treatment, Rick returned to South Riverdale Community Health Centre to hear the news he had been waiting for: he had been cleared of hepatitis C.

Rick also joined the program’s Continuing Care Group for those who have successfully completed their treatment and wish to remain connected with other participants who would like to pursue other health care goals. The group meets weekly for lunch and offers a range of social outings and trainings for members.
Clearing hepatitis C has given Rick the confidence that he can achieve similar outcomes in other aspects of his life, such as securing more permanent housing. He joined the TCHCP’s peer training program and hopes to one day be employed as a community support worker.

The success of the Toronto Community Hep C Program
Core components of TCHCP’s success include:
- Meaningful involvement of people with lived experience of hepatitis C in program design, delivery and research
- Reducing the barriers and stigma for people who use substances and are living with hepatitis C
- Ensuring a people-centred approach that is grounded in the principles of harm reduction and in supporting psycho-social needs, in addition to clinical issues
- Embedding research, evaluation and education throughout the program.


